By Mary Cheffers MD
From JAMA’s Rational Clinical Exam: Does this patient have Community-Acquired Pneumonia?
Summary
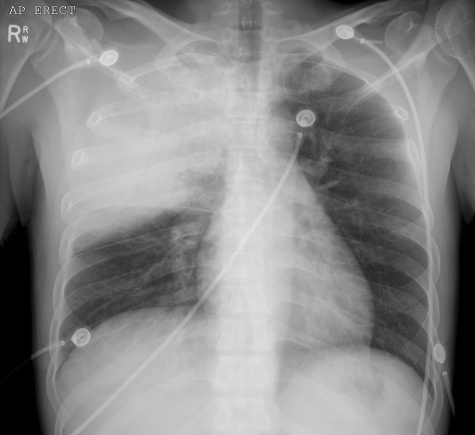
This is an old article, but the workup of Community-Acquired Pneumonia (CAP) in the ED has not changed significantly. The article sought to answer the question of whether a chest x-ray is necessary for a definite diagnosis in all patients with suspected CAP or if the H&P alone is sufficient. They conclude that clinical presentation is not sufficient. While there is no single element in the history or physical exam that can, by its presence or absence, obviate the need for a CXR to diagnose or exclude CAP, a combination of certain factors could increase your suspicion enough that a negative CXR would not add diagnostic utility.
The specifics
Of elements in the history, the best performers were the presence of dementia (LR + 3.4), Fever (LR + 2.1), and immunosuppression (LR + 2.2). Other symptoms fall much lower, including cough (LR +1.8), night sweats, chills (LR +1.7, 1.6 respectively). Interestingly, the presence of asthma by history has a strong negative predictive value with a +LR of 0.1.
In terms of physical exam, the best performers were a documented fever (LR + at 4.4) and tachypnea (LR +3.4). Presence of crackles, bronchial breath sounds, or tachycardia all have a similarly low LR+, around 2. Notably, the absence of pathologic lung findings only has an LR – of 0.57, whereas the absence of any vital sign abnormalities is quite useful with a LR – of 0.18.
Combining the top performing factors moderately improves their diagnostic utility. The prediction rule created by Diehr et al. uses a point system, weighting fever, tachypnea, sputum, myalgias, and night sweats. A score of 3 yields an LR+ of 14.
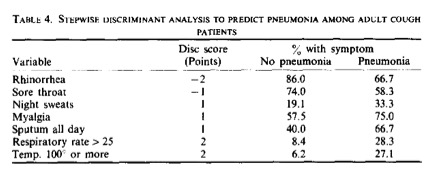
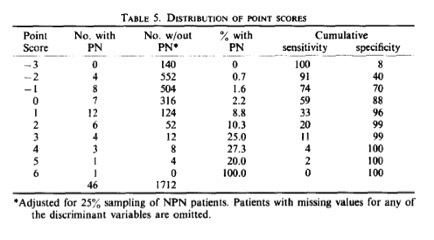
Diehr P, Wood RW, Bushyhead J, Krueger L, Wolcott B, Tompkins RK. Prediction of pneumonia in outpatients with acute cough: a statistical approach. J Chronic Dis. 1984;37(3):215-225
In the ED, if we were to use an estimated prevalence of 15%, using Diehr’s system, a score of 3 would give your patient a 70% chance of having CAP. This would suggest that in an ED setting, the presence of multiple clinical factors suggestive of CAP makes a negative CXR (with a quoted sensitivity of 43%) a poorer test than the clinical presentation.
Take away points
In the end, given that the mortality of CAP seen in the ED is relatively high (15% for those we are admitting to wards, and almost 40% for those who merit ICU admission), it makes sense to (1) have a low threshold to do a CXR since it has a high specificity and (2) not to discount CAP in a patient in whom you have a high clinical suspicion and a negative CXR.
Sources
Joshua P. Metlay, MD, PhD; Wishwa N. Kapoor, MD, MPH; Michael J. Fine, MD, MSc.
The Rational Clinical Exam: Does This Patient Have Community-Acquired Pneumonia? Diagnosing Pneumonia by History and Physical Examination. JAMA. 1997;278(17):1440-1445. doi:10.1001/jama.1997.03550170070035.
Diehr P, Wood RW, Bushyhead J, Krueger L, Wolcott B, Tompkins RK. Prediction of pneumonia in outpatients with acute cough: a statistical approach. J Chronic Dis. 1984;37(3):215-225
Wesley H. Self, MD MPH, D. Mark Courtney, MD MSCI, Candace D. McNaughton, MD MPH, Richard G. Wunderink, MD, and Jeffrey A. Kline, MD. High Discordance of Chest X-ray and CT for Detection of Pulmonary Opacities in ED Patients: Implications for Diagnosing Pneumonia. Am J Emerg Med. 2013 Feb;31(2):401-5