By Mary Cheffers, MD
The background:
- Non-hemorrhagic hypovolemia is commonly classified as “mild” (3-5%), “moderate” (6-9%) and “severe” (>10%)
- The level of dehydration in children is important, since you can attempt to orally rehydrate those with mild dehydration, avoiding the pain and expense related to IV hydration, while undiagnosed severe dehydration may lead to morbidity or mortality
- The assessment of dehydration can be separated into signs of either tissue desiccation (dry mucous membranes, skin turgor) or compensatory reactions to maintain vital perfusion (capillary refill time, low urine output)
So what can I rely on to help me recognize dehydration and distinguish between mild and severe?
The quick answer:
- No individual sign is reliable, but the best 3 individual examination signs for assessing dehydration are:
- prolonged capillary refill time
- abnormal skin turgor
- abnormal respiratory pattern
- Groups of signs or use of clinical scales improves diagnostic characteristics
- A normal bicarbonate concentration helps somewhat to reduce the likelihood of dehydration
Will a decision tool help me?
In 1997, Gorelick et al. created an evidence-based scale intended to be used as a prediction tool for pediatric dehydration. Although this tool was created many years ago, it remains useful today as the data on which it was based still endures. In their model, the practitioner assesses 10 physical exam findings weighted equally (interestingly, a sunken anterior fontanelle is not a criterion).
Having 3 or more signs present in your patient yields an LR of 4.9 that the child is at least 5% dehydrated. The presence of 7 or more of the 10 signs in your patient gives an LR of 8.4 that the child is severely (at least 10%) dehydrated.
Is there a scale that I would actually use in the ED?
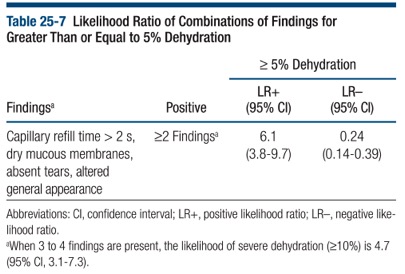
A simplified version of this scale takes 4 of the most predictive elements and weighs them equally:
- capillary refill time
- dry mucous membranes
- absence of tears
- abnormal overall appearance
If a child demonstrates 2 of these 4 elements there is a LR of 6.1 to predict at least 5% dehydration. The presence of 3 findings offers an LR of 4.7 for severe dehydration (>10%).
If only one or none of these findings are present, there is an LR(-) of 0.24 for 5% dehydration, making it a useful quick assessment tool.
By incorporating one or more of these evidence-based tools into practice, the clinician can more confidently and appropriately diagnose and treat pediatric dehydration.
References:
Steiner, DeWalt, Byerley. Is This Child Dehydrated? Ch. 25 in JAMA Rational Clinical Exam. 2009
Gorelick MH1, Shaw KN, Murphy KO. Validity and reliability of clinical signs in the diagnosis of dehydration in children. Pediatrics. 1997 May;99(5):E6.